Don’t Be Surprised When You Get Omicron
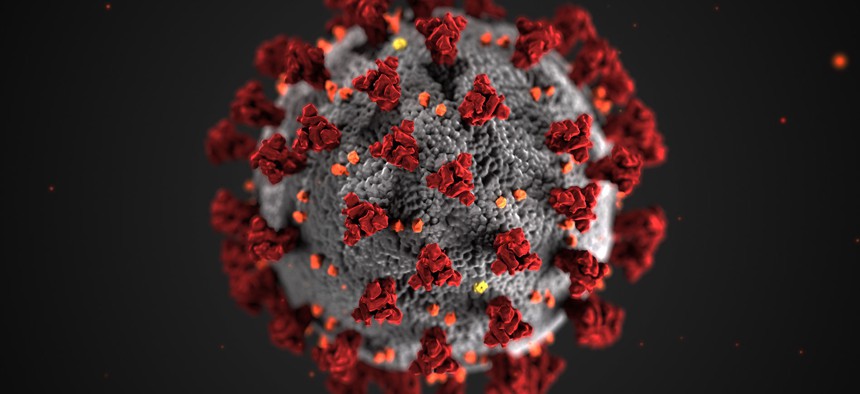
CDC
America is in for a lot more breakthrough infections. Here’s what to do if you fall sick.
My breakthrough infection started with a scratchy throat just a few days before Thanksgiving. Because I’m vaccinated, and had just tested negative for COVID-19 two days earlier, I initially brushed off the symptoms as merely a cold. Just to be sure, I got checked again a few days later. Positive. The result felt like a betrayal after 18 months of reporting on the pandemic. And as I walked home from the testing center, I realized that I had no clue what to do next.
I had so many questions: How would I isolate myself in a shared apartment? And why for 10 days, like the doctor at the testing site had advised? Should I get tested again? Following the doctor’s orders, my partner—who had tested negative—dragged a sleeping bag to the couch. Masks came on, windows went up, and flights were canceled. I ate flavorless dinners on my side of the apartment. One by one, the symptoms I knew so well on paper made their real-life debut: cough, fever, fatigue, and a loss of smell so severe, I couldn’t detect my dog’s habitually fishy breath.
Turns out I wasn’t the only one feeling baffled about what to do. “Oh yeah, people are very confused about breakthrough cases,” Peter Chin-Hong, an expert on infectious diseases at UC San Francisco, told me. Now that the Omicron variant is here, many more Americans may soon have to deal with breakthrough confusion. There’s a lot we don’t know about the new variant, but it’s spreading fast. Although the unvaccinated remain most at risk, vaccinated America isn’t in the clear: While the shots still seem effective at preventing hospitalization and death, early reports suggest that they are less effective against milder cases. So if you do get a breakthrough infection right now, what should you do?
[Read: The pandemic of the vaccinated is here]
At least for now, Omicron shouldn’t change how Americans act when they get a breakthrough infection. “All of the same things stand, whether it’s Delta, Omicron, or any other Greek letter or non-Greek letter of SARS-CoV-2,” says Stephen Kissler, an epidemiologist at Harvard. “Once you know you’re infected, hang tight, limit your encounters with other people, and just take care of yourself.”
If only the official guidance were this straightforward. Rebecca Wurtz, an infectious-disease expert at the University of Minnesota, told me that people are perplexed “partly because, I think, the guidance is confusing.” The CDC’s guidelines are limited: Isolate if you’ve either tested positive in the past 10 days or are experiencing symptoms, and end your isolation after 10 days only if you’ve gone 24 hours with no fever (without the use of Tylenol or other anti-fever drugs) and your other symptoms are improving—not counting the loss of taste and smell, which could take a couple of weeks to return. “They’re unclear as they’re stated, and they’re a little too complicated in any case,” Wurtz said. (When I reached out to the CDC for comment on its guidance on breakthroughs, a spokesperson pointed me back to the recommendations on the agency’s website.)
If you start feeling anything that resembles COVID symptoms or learn that you’ve been exposed to someone who has tested positive, some experts told me, the first thing to do is to get tested. “If you’re not sure, you have to get tested,” Chin-Hong said. That’s especially true now that we’re heading into the winter, when all sorts of non-COVID illnesses are also circulating. It can be impossible to differentiate between the early symptoms of a cold, the flu, and COVID, and getting tested is the only way to confirm a breakthrough infection. The bottom line is that knowing whether you’re positive is important not just for you, but also for anyone who you’ve been in contact with recently—especially those who are unvaccinated or immunocompromised.
PCR tests are still considered to be the gold standard, but they take much longer to generate results than rapid tests, which you can buy at a pharmacy and take at home. A test is merely a snapshot in time, and because Omicron appears to have a shorter incubation period than past variants, a result from a few days ago may not mean much. More than 60 fully vaccinated people tested positive for Omicron after an office holiday party in Norway, and all had gotten negative rapid-test results just a day earlier.
[Read: Omicron’s explosive growth is a warning sign]
Wurtz said that if you start to feel sick but haven’t been in contact with anyone and don’t plan to be, the best recourse is to stay home, minimize exposure to other people, and rest. “This may seem a little radical,” she said, “but I don’t think there’s a need in that context to be tested at all, period.” Again, the thing to consider is whether you’ve put anyone around you at risk of infection.
If you do test positive, you should alert your local public-health authority so they can initiate contact tracing, Chin-Hong said. Many testing sites do this automatically, but at-home tests, of course, do not. The CDC advises that after confirming your infection, you should start isolating right away, but unless you are asymptomatic, the first day of symptoms is technically what counts as the start of your 10 days of isolation. I learned the hard way that you aren’t supposed to “test out” of isolation, when a physician assistant yelled at me for getting tested after feeling better on day seven. She said I was putting others at risk, although the CDC guidance didn’t specifically say not to get tested. Explaining that I would have to isolate regardless of the outcome, she never told me my result.
Isolating can be especially tricky if, like many Americans, you don’t get paid sick leave, or if you live with people who have tested negative. That’s a common situation with breakthrough infections: While a positive test in a household full of unvaccinated people may soon lead everyone to test positive, that’s not necessarily the case in a home where everyone is vaccinated. “At the minimum, don’t be in the same room,” Javaid said. “If you have to interact with each other, you should always wear masks.” Considering Omicron’s contagiousness, it’s worth wearing more protective masks, such as N95s or KN95s, in lieu of the cloth masks that are common across the U.S. And even if it’s cold, opening windows four to six inches, Kissler said, can help with ventilation. If people you live with start having symptoms, the same guidelines apply: They too should self-isolate, and test if they’re going to see others.
But as The Atlantic’s Katherine Wu has written, not all public-health experts agree that those with breakthrough infections really need to isolate for 10 days, given recent research suggesting that they clear the virus more quickly than the unvaccinated, for whom the 10-day window was designed. Wurtz said that the 10-day isolation period is “somewhat arbitrary,” but she acknowledged that the cautiousness can be reassuring with a new, less understood variant.
Thankfully, most breakthrough infections tend to be mild cases, and that seems likely to hold true with Omicron too (especially for those with booster shots). If you’re feeling unwell, the usual treatment for respiratory infections—cold-and-flu medications, anti-fever drugs, liquids, and rest—are sufficient for most people with breakthrough COVID, Wurtz said. Although monoclonal antibodies are effective at treating COVID, Chin-Hong said he offers them only to people who are older or immunocompromised, because they are the most vulnerable, even after getting vaccinated. (Soon, we’ll have yet another treatment option: antiviral pills.) Breakthrough infections are unlikely to lead to hospitalization for most people, but you should seek emergency care if you develop any severe symptoms, such as trouble breathing, persistent pain or pressure in the chest, or confusion.
[Read: Timing is everything for Merck’s COVID pill]
At some point, as we learn more about Omicron, the guidance regarding what to do after getting a breakthrough infection could change. “I think it’s important with the new variant that we’re seeing right now to consider getting the boosters as soon as possible,” Javaid said. But aside from that, the best thing vaccinated people can do is make sure they’re ready for a breakthrough infection before it strikes. Stock up on rapid tests so you’re not in a bind if any COVID symptoms suddenly appear. Talk to your family or roommates about where the best place to isolate is in your home. Be prepared to miss 10 days of work if you’re in person.
Thankfully, I’m fully recovered from my breakthrough infection, except for the ongoing inability to smell my dog’s breath. For now, what makes breakthroughs like mine so confusing is that the U.S. is in an “awkward transition phase,” Wurtz said, between following somewhat random rules—such as isolating for 10 days—and more deeply understanding what COVID-19 does to our bodies. I’ve since gotten a booster, and accepted that I’ll probably get sick with COVID again, maybe many times. COVID will someday turn endemic, and having it may become more like having a cold or a bout of flu: a normal, albeit exasperating, part of everyday life for most people (though not everyone). Eventually, even with Omicron, breakthroughs will become a lot less stressful. “I do think it is time to start normalizing breakthrough infections,” Wurtz added. “We have to learn to live with them.”
This article was originally published in The Atlantic. Sign up for their newsletter.





