This 3-D Printer Creates Human Muscles and Tissues That Could Actually Replace Real Ones
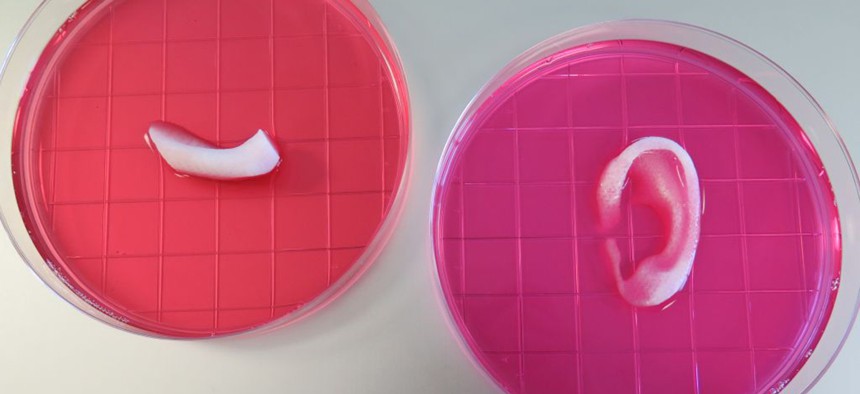
A piece of 3D-printed jawbone and ear cartilage. Wake Forest Institute for Regenerative Medicine
Unlike with most printers, which put down layers of molten plastic or metal, Wake Forest’s printer lays down what are called hydrogels—water-based solutions containing human cells.
We’re getting closer to the plug-and-play human body.
Researchers at Wake Forest University in North Carolina say they have created a 3-D printer that can produce organs, tissues and bones that could theoretically be implanted into living humans. The group’s work was published in the scientific journal Nature Biotechnology today.
According to the paper, the researchers’ printer acts much like most 3-D printers do, using a computer-controlled nozzle to extrude layers of materials in a very precise pattern. The layers eventually harden to produce whatever you’re trying to print. But unlike with most printers, which put down layers of molten plastic or metal, Wake Forest’s printer lays down what are called hydrogels—water-based solutions containing human cells.
The university’s printer has multiple nozzles, some extruding hydrogels, others biodegradable materials that are used to give the tissue it’s printing structure and strength. When the supporting materials dissolve and tissue finishes incubating in the machine, it could be potentially implanted into a person.

The researchers ran three-dimensional scans on human ears, jawbones and muscles to create digital templates for their printer. They then printed out an ear-shaped piece of cartilage, a muscle and a piece of a jawbone, and implanted them in mice. The structure of the university’s printer allows it to print out tissues that can accommodate blood vessels, meaning they can receive the oxygen and nutrients that cells need to survive. This has been a sticking point for many of the 3-D printers that have tried to print living tissue in the past. According to the paper, the school’s printed products showed no signs of necrosis, or cells dying in the tissue.
“Future development of the integrated tissue-organ printer is being directed to the production of tissues for human applications, and to the building of more complex tissues and solid organs,” lead researcher Anthony Atala told Quartz. “When printing human tissues and organs, of course, we need to make sure the cells survive, and function is the final test. Our research indicates the feasibility of printing bone, muscle and cartilage for patients. We will be using similar strategies to print solid organs.”

It’s worth noting that the Wake Forest researchers aren’t the only ones researching bioprinting like this. Todd Goldstein, a researcher at the Feinstein Institute for Medical Research at Northwell Health, told Quartz that “this isn’t completely novel.”
Goldstein is currently working on 3-D printing human cells to use in implantable tracheas. But he said the research’s true novelties lie in the fact that it’s combined the entire process into one machine, and the quality of the results it’s getting. He suggested thinking of it this way: “If you have a really good baker that can come up with an amazing seven-layer cake—he has no new ingredients, but the way they put it together made it taste really good.”
A Philadelphia-based startup, BioBots, released a $10,000 3-D printer in September that prints human tissue. The company’s CEO, Danny Cabrera, told Quartz that Atala is on BioBots’ scientific advisory board.
“Nothing’s totally different here," Cabrera said, “the main difference is that this one has four heads.”
While it’s become increasingly apparent that 3-D printing hasn’t proven overly useful for the average consumer, it’s showing real promise in other areas. The first 3-D-printed drug was approved for use by the U.S. Food and Drug Administration last August, and doctors in Spain managed to successfully install a 3-D-printed titanium ribcage on a patient in September.
It remains to be seen whether Wake Forest’s printed organs—or anyone else’s—will be tested on actual humans anytime soon. The researchers said in their paper that their technology would require “further development” before its organs could be tested on a human. FDA previously told Quartz that it has not approved any 3-D printers for any internal human use, but it has “significant scientific interest in this topic.”
The logical conclusion of bioprinting research, if found safe sand reliable, could well be to dramatically reduce the wait-time for transplants, and perhaps even replace humans’ healthy organs with even better ones. It’s something that Martine Rothblatt, the founder of SiriusXM, is also trying to solve. Rothblatt “has to my knowledge a perfect track record in making [her] visions real,” Google futurist Ray Kurzweil told The Washington Post. But for now, and for the near future, the tens of thousands of people waiting for a transplant will just have to keep hoping their number is up next.
NEXT STORY: The Military’s Superfast Bird Drone





