Deer, Mink and Hyenas Have Caught COVID-19 – Animal Virologists Explain how to Find the Coronavirus in Animals and why Humans Need to Worry

adogslifephoto/istockphoto
COVID-19's spread in animals could pose major problems for people, too.
In April 2020, tigers and lions at the Bronx Zoo made the news when they came down with COVID-19. In the months following these surprising diagnoses, researchers and veterinarians found SARS-CoV-2, the virus that causes COVID-19, in nearly a dozen other species, both in captivity and in the wild.
How are so many animals catching the coronavirus? And what does this mean for human and animal health?
We are veterinary researchers who investigate animal diseases, including zoonotic diseases that can infect both humans and animals. It is important, for both human and animal health, to know what species are susceptible to infection by the coronavirus. Our labs and others across the world have tested domestic, captive and wild animals for the virus, in addition to conducting experiments to determine which species are susceptible.
The list of infected animals so far includes more than a dozen species. But in reality, infections may be much more widespread, as very few species and individual animals have been tested. This has real implications for human health. Animals can not only spread pathogens like the coronavirus, but also can be a source of new mutations.
Which animals have caught the coronavirus?
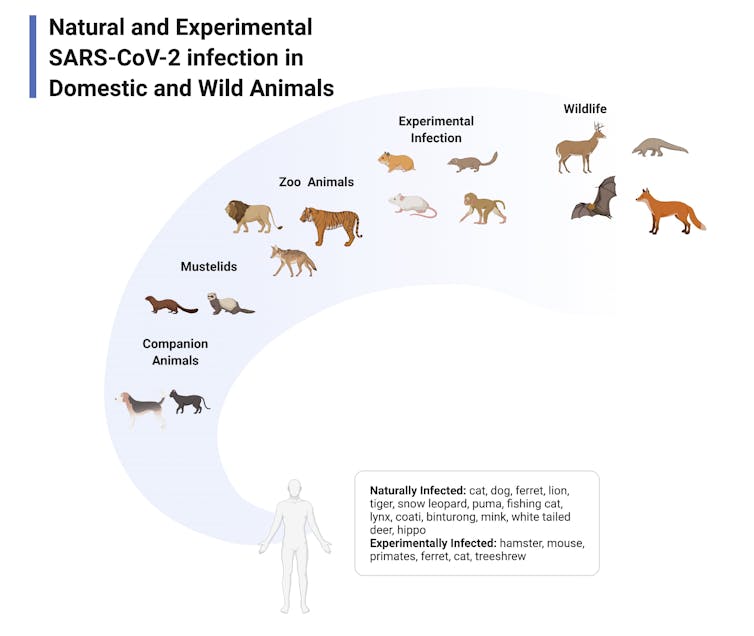
As of February 2022, researchers and veterinary diagnostic labs have confirmed that 31 species are susceptible to SARS-CoV-2. In addition to pets and zoo animals, researchers have found that a number of nonhuman primates, ferrets, deer mice, hyenas, wood rats, striped skunks and red fox are among the animals that are susceptible to infection by SARS-CoV-2.
White-tailed deer and mink are the only two species of animals that have been found harboring the virus in the wild. Fortunately, most animals don’t appear to experience clinical disease like humans do, with the exception of mink. However, even animals that don’t appear sick may be able to transmit the virus to each other and, potentially, back to people. Still unanswered are many questions about which animals can contract the virus and what, if anything, that means for people.

How to look for a virus in animals
There are three ways to study zoonotic diseases: by looking at pets or captive species like animals in zoos, testing wild animals for the coronavirus or by exposing animals to the virus in a lab.
During early stages of the pandemic, when a few pet owners or zoo caretakers observed animals with breathing problems or coughing, they arranged with veterinarians to get them tested for the coronavirus. The U.S. Department of Agriculture and the Centers for Disease Control and Prevention coordinate COVID-19 testing and management in animals. The same process of taking a sample and running it through a PCR machine to test for the coronavirus works just as well for animals as it does for people, though swabbing the nose of a lion – or even a pet cat – requires a bit more training and finesse. Veterinary diagnostic laboratories like our own run hundreds of thousands of tests for animal diseases each year, so we were able to easily begin testing for SARS-CoV-2.
Relying on previous research, scientists have been able to make some guesses as to which animals are susceptible and have been testing these hypotheses. Cats, hamsters and ferrets were all infected during the first SARS outbreak in 2002, so researchers suspected they would be susceptible to the new coronavirus. Sure enough, research showed that SARS-CoV-2 readily infected these species in laboratory experiments. Mink are closely related to ferrets, and during the summer and fall of 2020, mink farms across the U.S. became sites of huge outbreaks after people passed the coronavirus to the animals.
Using computer models, scientists were also able to predict that the coronavirus could easily infect some species of deer using key proteins on their cells. Based on these predictions, researchers began testing white-tailed deer for the coronavirus and first reported positives in August 2021.
Most recently, on Feb. 7, 2022, researchers published a preprint paper showing that deer on Staten Island, New York, are infected with the omicron variant. Since this is the virus infecting most New Yorkers, this provides strong evidence that humans somehow transmitted the virus to deer. How deer in at least six states and Canada initially came in contact with SARS-CoV-2 remains a mystery.
Finally, to understand how the coronavirus affects animals, researchers have been conducting carefully controlled exposure experiments. These studies evaluate how infected animals shed the virus, whether they have clinical symptoms, and whether and how much the virus mutates in different species.
Risks of a species-jumping coronavirus
The risk of contracting SARS-CoV-2 from an animal is, for most people, far lower than being exposed to it by another human. But if the coronavirus is living and spreading among animals and occasionally jumping back to humans, this process – known as spillover and spillback – poses its own threats to public health.
First, infection of animals simply increases the concentration of SARS-CoV-2 in an environment. Second, large populations of animals that can sustain the infection can act as a reservoir for the virus, maintaining it even if the number of infections in humans decreases. This is particularly concerning with deer that live in high numbers in suburban areas and could transmit the virus back to people.
Finally, when SARS-CoV-2 spreads from humans to animals, our laboratory’s own work indicates that the virus very rapidly accumulates mutations. Viruses adapt to the unique characteristics – body temperature, diet and immune composition – of whatever animal they are living in by mutating. The more species infected, the more mutations occur. It’s possible that the new variants emerging in people could infect new animal species. Or it’s possible that new variants could initially arise from animals and infect humans.
The story of SARS-CoV-2 in animals isn’t over yet. According to the CDC, six of every 10 human infectious diseases can be spread from animals to people, and around three-quarters of new or emerging infectious diseases in people come from animals. Research has shown that investing in the study of zoonotic diseases could vastly reduce the costs of future pandemics, and this type of complex research has historically been underfunded. Yet despite this, in 2021, the CDC allocated only $193 million toward the study of emerging zoonotic infectious diseases – less than a quarter of 1 percent of the CDC’s total budget.
There are still many unknowns about how viruses transfer between humans and animals, how they live and mutate in animal populations and the risks of species-jumping viruses. The more researchers know, the better health officials, governments and scientists can prepare and prevent the next pandemic.
[Research into coronavirus and other news from science Subscribe to The Conversation’s new science newsletter.]
![]()
Sue VandeWoude, University Distinguished Professor of Microbiology, Immunology, and Pathology and Director of the One Health Institute, Colorado State University; Angela Bosco-Lauth, Assistant Professor of Biomedical Sciences, Colorado State University, and Christie Mayo, Associate Professor of Microbiology, Immunology and Pathology, Colorado State University
This article is republished from The Conversation under a Creative Commons license. Read the original article.





