The Next Frontier for 3-D Printing: Human Organs
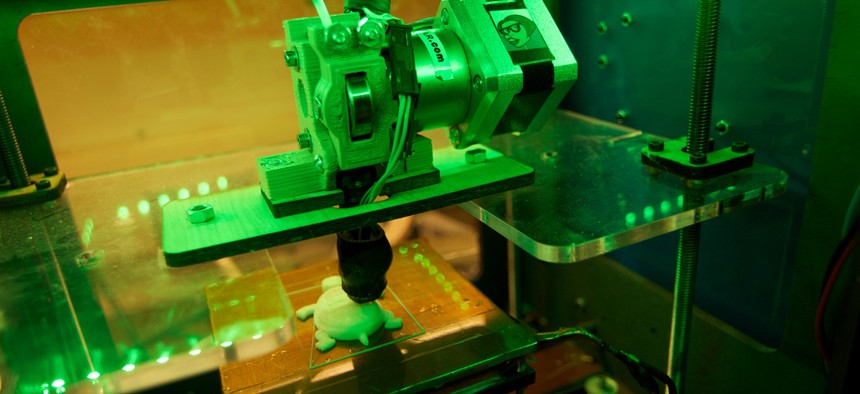
Flickr user kakissel
The technology also is being used to test drug responses in mini-systems.
Researchers at Wake Forest Baptist Medical Center are embarking on a project that is so overloaded with sci-fiesque elements that if it were a movie, you might question the screenwriter's credibility.
The "body on a chip" project will use 3-D printing—or bioprinting—technology to create mini human-organ systems about the size of a quarter to test the body's response to drugs. It's funded by a $24 million grant from the Defense Department to develop antidotes to very strong agents in the areas of chemical and biological warfare.
The ultimate goal of bioprinting is to create large, functional, implantable organs that will address the growing gap between viable organ supply and demand for transplants. Along the way, the simpler, mini-versions can be used to more effectively test drugs.
A few groups have been experimenting with bioprinting tissues and organs, but the body-on-a-chip project is unique in connecting the structures together. The chip will be able to test the impact of agents—including intense chemical weapons, more mainstream drugs, and treatments—on the human body. The project offers an alternative to animal testing—which is often inefficient and inaccurate for measuring human responses—and enables the lab to test the full system's response, rather than just one type of organ.
Scientists started making tissues by hand about 25 years ago. Using a technique known as scaffolding, cells from a patient's tissue were layered on 3-D molds and grown in an incubator outside the body. Using bioprinting technology, they are now able to feed the same information into a computer to build the tissue.
"Printing came about as a way to scale up the tissues and organs we were already creating by hand," says Anthony Atala, director of the Wake Forest Institute of Regenerative Medicine in North Carolina and the lead investigator on the project. Bioprinting enables researchers to create tissues with much greater precision and accuracy.
Atala explains the four tissues types in order of complexity: Simplest are flat structures like skin; second are tubular structures, such as blood vessels or windpipes; third are hollow non-tubular organs, such as the stomach, bladder, and uterus; and last and most complex by far are solid organs, such as the heart, kidney, and liver. These have more cells per area, more cell types, and higher nutrition requirements, and they need much more vascularity and blood supply.
To this point, scientists have only implanted the first three types from handmade tissues in patients. No bioprinted structure has been implanted.
The mini-organs are small enough that they don't require a complex vascular tree to survive. The mini-livers, hearts, lungs, and kidneys are not fully functional native organs, but they mimic the functionality for the testing application.
The Wake Forest lab has developed one machine to bioprint different types of tissues. "It's like with an inkjet printer, where you have different colors," says Sang Jin Lee, a coinvestigator on the project. "Here we have different nozzles and different materials and cells."
The researchers are borrowing from computer microchip and biosensing technology. They will focus on one organ type at a time, beginning with the liver. As each is developed, it will be used to test drug responses individually; once they are completed, they will be connected on the chip to test the full system response.
A small handful of other groups are developing technologies to print tissues, although generally with a focus on individual organs, rather than the full system.
Organovo, a start-up in San Diego, is using bioprinting of tissues to improve research on drugs, with a recent focus on the liver.
"Reliance on animal models and cells in a petri dish [for testing] is problematic, because many diseases can't get good animal models or don't behave similarly in petri dishes," says Organovo CEO Keith Murphy. The company has succeeded in bioprinting liver tissue that lasted 40 days in a dish. Murphy says normally the tissue stops functioning in two days, which is not helpful for testing a drug that is administered for two years.
Organovo is focused on the immediate commercial impact of bioprinting, with testing done on each tissue independently. "We've contemplated putting [the parts] together over time, but you don't need 10 things to study the liver—you need the liver," explains Murphy.
"You can make living structures act like living tissues," he says. "You don't need the full organ to have an impact."
The Advanced Manufacturing Technology Group at the University of Iowa is bioprinting tissue with this idea in mind. Ibrahim Ozbolat, AMTech codirector and assistant professor of mechanical and industrial engineering, is focused on creating tissue that would accompany—not necessarily replace—the pancreas and produce insulin to help patients with diabetes.
"We're not interested in making a full natural pancreas," he says. "We're working on making something that is large enough and produces enough insulin that is transplantable."
These projects are all steps along the path toward bioprinting large organs, although that goal and its clinical application is years in the future.
"[Bioprinting organs] is still several billion dollars away," Murphy says. "If the funding is provided in five years, it could happen quickly. If it takes 20 years, it will be more over that time frame."
The hope is that as the technologies continue to develop, the manufacturing of organs could help solve the problem of rapidly growing transplant wait-lists.
Atala notes that over two sets of 10 years, the number of patients on wait-lists has doubled, while the number of organs transplanted has increased by only 1 percent—a problem the American Hospital Association has declared a public health crisis.
"This is really what drives us to do this," he says. "Everything builds on the next step."
(Image via Flickr user kakissel)






